🍁Greetings to one and all going through my E log!!
🩺This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment.
I am Nomika Alli (Roll no 179) of 9th Sem MBBS.
A 67 year old Male R/O Devarakonda , came to the casualty on 2nd December 2023 with complaints of Shortness of breath since 10 days and pedal & facial edema since 8 days
HISTORY OF PRESENT ILLNESS:
Patient came in drowsy but arousable state to the casualty . He was apparently asymptomatic 10 days back , then he developed Shortness of breath which is insidious in onset, gradually progressive in nature, aggravating on exertion and relieved on taking rest, progressed from grade II to grade III- IV (Modified MRC)
Orthopnea, Paroxysmal nocturnal dyspnea present
C/O Bilateral pedal edema below knees , facial puffiness and periorbital edema since 8 days , insidious onset, gradually progressive in nature , no diurnal variation, pitting type I.
C/o decreased urine output and decreased appetite since 5days
No C/o chest pain, palpitations, profuse sweating,
No c/o fever, cold, cough, nausea, vomiting, loose stools.
His daily routine is waking up at 6: 00 am, breakfast as idli/upma at 8:00 am . He used to have his lunch as rice and curry , sambhar/rasam at 1: 00 pm .He usually haves his dinner as chapati/upma/rice and curry at 8:00pm and goes to bed by 9:00 pm.The patient used to lead a normal life before this 15days .
HISTORY OF PAST ILLNESS:
K/c/o asthma since 10yrs -on medication
N/K/C/O DM, CAD, CVD, Thyroid, epilepsy
K/C/O HTN 6 yrs ago and used medication for 3 yrs and stopped as BP was under control
H/O TB 30 yrs ago
SURGICAL HISTORY: -
FAMILY HISTORY:
N/K/C/O DM, HTN, Asthma, Epilepsy, CAD, CVD, TB, Thyroid
PERSONAL HISTORY:
Married
Shop keeper by occupation
Diet: Mixed
Appetite: decreased
Sleep: adequate
Urine output decreased
Bowel movements: Regular
Addictions: Alcohol occasionally
Allergies: no known
GENERAL EXAMINATION:
Patient is drowsy due to sedation, coherent to time , place, person.
Ht: 155cm Wt: 58 kg
Pallor: present
Icterus: absent
Clubbing: absent
Cyanosis: absent
Koilonychia: absent
Lymphadenopathy: absent
Post intubation vitals: Vitals: Temp: 98 F
BP: 90/60 mmHg
PR: 102 bpm
RR: 15 cpm ACMV mode
SpO2: 100% at 5 litre O2
GRBS: 126 mg%
SYSTEMIC EXAMINATION:
RS:
Orthopnea +
Paroxysmal nocturnal dyspnoea +
wheeze +
Central position of trachea
NVBS +
CVS:
S1 S2 heard
No murmurs
No thrills
ABDOMEN:
Shape of abdomen: mildly distended
No tenderness
No palpable mass
No bruits
Liver and spleen- not palpable
Bowel sounds heard
CNS:
drowsy but arousable
no neck stiffness
kernig's sign negative
cranial nerves: normal
motor - intact
sensory - intact
Glasgow scale E2V2M2 = 6/15
MUSCULOSKELETAL SYSTEM: normal
SKIN: normal
ENT: normal
TOOTH & ORAL CAVITY: normal
PHYSICAL EXAMINATION:
muscle wasting++
PROVISIONAL DIAGNOSIS:
Altered sensorium ? AKI ??
HEART FAILURE(ET 51%)
ANAEMIA
INVESTIGATIONS:
2-12-23
RFT raised urea, creatinine, uric acid, phosphorus,
V

ABG
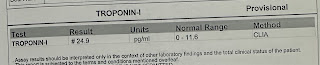
TROPONIN ↑
BLOOD UREA ↑↑
S. Creatinine ↑ ↑
potassium ↑
blood sugar↑
LFT: AST, Alkaline phosphatase, total proteins↑
RFT: Urea, creatinine, phosphorus, potassium ↑
USG
ECG: Left ventricular hypertrophy
MRI Brain plain
The patient may be having (from investigations)
UREMIC ENCEPHALOPATHY
AKI ON CKD
HEART FAILURE EF 51%
Anemia secondary to CKD
TREATMENT:
intubated i/v/o respiratory failure & low GCS
IV fluids NS @50ml/hr
Ryles feeds water 50ml 2hrly milk 100ml 3hrly
Inj. midazolam 30ml= Inj. Fentanyl
Inj. Noradrenaline 2amp
Inj. Piptaz 2.25ml IV/TID
ET Tube suction 2hrly
chest physiotherapy
position change 2hrly
monitor vitals hrly
Tab. Aspirin
Tab. atorvastatin
3-12-23
APTT
PT
Hemogram: low HB , lymphocytes, eosinophils, PCV, RBC count
raised total count, neutrophils
BT& CT
ABG
RFT: Raised urea, creatinine
ECG
The patient may be having (from investigations)
UREMIC ENCEPHALOPATHY
AKI ON CKD
HEART FAILURE EF 51%
Anemia secondary to CKD
TREATMENT:
intubated i/v/o respiratory failure & low GCS
IV fluids NS @50ml/hr
Ryles feeds water 50ml 2hrly milk 100ml 3hrly
Inj. midazolam 30mg+ Inj. Fentanyl 200mcg @16mg/hr
Inj. Piptaz 2.25gm IV/TID
ET Tube and oral suction hrly
Tab. Nodosis 500mg
chest physiotherapy
position change 2hrly
monitor vitals hrly
Tab. ecosprin 75mg RT/OD
Tab. atorvastatin 20mg
4-12-23
2D ECHO:
- No RWMA, paradoxical IVS
- trivial MR, Mild AR
- mild to moderate TR with PAH
- Sclerotic AV, no AS/MS, IAS- intact
- EF= 51 RVSP2 48mmHg
- Good LV systolic function
- diastolic dysfunction
- mild PE(+)
- IVC size 1.20cm collapsing
ABG
Hemogram: low HB , lymphocytes, PCV, RBC count
raised total count, neutrophils
RFT :Urea, creatinine raised
ECG
The patient may be having (from investigations)
UREMIC ENCEPHALOPATHY ??
AKI ON CKD
HEART FAILURE EF 51%
Anemia secondary to CKD
TREATMENT:
intubated i/v/o respiratory failure & low GCS
IV fluids NS @50ml/hr
Ryles feeds water 50ml 2hrly ,milk 100ml 3hrly
Inj. midazolam 30mg+ Inj. Fentanyl
Tab. Nodosis 1gm
Inj. Piptaz 2.25ml IV/TID
ET Tube and oral suction hrly
chest physiotherapy
position change 2hrly
monitor vitals 4 hrly
I/O charting
Tab. ecosprin 75mg
Tab. atorvastatin 20mg
Inj. lasix 40mg
Inj.KCl 40mcg in 500ml/NS
5-12-23
ABG
ECG
The patient may be having (from investigations)
UREMIC ENCEPHALOPATHY ??
AKI ON CKD
HEART FAILURE EF 51%
Anemia secondary to CKD?
TREATMENT:
intubated i/v/o respiratory failure & low GCS
IV fluids NS & DNS@50ml/hr
Ryles feeds water 50ml 2hrly ,milk 100ml 3hrly
Inj. Piptaz 2.25ml IV/TID
Inj. sodium bicarbonate 20ml/IV/TID
ET Tube and oral suction 2hrly
monitor vitals hrly
I/O charting
Tab. ecosprin 75mg
Tab. atorvastatin 20mg
Inj. lasix 40mg
Inj. KCl 40mcg in 500ml/NS
Tab. shelcal ct
Tab. orofer xt
12
6-12-23
Hemogram: low Hb, lymphocytes, eosinophils, PCV, RDC count
RFT: raised urea, Creatinine
ABG
The patient may be having (from investigations)
UREMIC ENCEPHALOPATHY ??
AKI ON CKD
HEART FAILURE EF 51%
Anemia secondary to CKD?
TREATMENT:
intubated i/v/o respiratory failure & low GCS
IV fluids NS & DNS@50ml/hr
Ryles feeds water 50ml 2hrly ,milk 100ml 3hrly
Inj. Piptaz 2.25ml IV/TID
Inj. sodium bicarbonate 20ml/IV/TID
ET Tube and oral suction 2hrly
monitor vitals hrly
position changing 2hrly
I/O charting
Tab. ecosprin 75mg
Tab. atorvastatin 20mg
Inj. lasix 40mg
Inj. KCl 40mcg in 500ml/NS
Tab. shelcal ct
Tab. orofer xt
inj. pantop 40mg
inform sos
References:


.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)













































.png)

