🍁Greetings to one and all going through my E log!!
🩺This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment. I am Nomika Alli (Roll no 179) of 6th Sem, MBBS.
A 20 yr old female came to OPD on 20-12-2022 4:36 pm with chief complaints of left low Back ache radiating to umbilicus since 4 days, vomiting since one half day and loose stools since one day.
HISTORY OF PRESENT ILLNESS:
This patient is a 20 yr old female, B.Sc. Nursing student by occupation. The pt. was apparently asymptomatic 4 days back, then she developed low back pain radiating to umbilicus C/O one episode of vomiting which was non projectile & contained food particles one half days ago . She had loose stools since 1 day which were 5-6 episodes per day ( non blood stained).
H/O food intake on Sunday (?? outside)
No H/O fever, SOB, Headache.
HISTORY OF PAST ILLNESS:
Not K/C/O DM/ HTN/ CVA/ CAD/ Epilepsy/ TB/ Asthma / thyroid
no blood transfusions
TREATMENT HISTORY:
not significant.
SURGICAL HISTORY;
not significant.
PERSONAL HISTORY:
- unmarried
- student by occupation
- appetite: normal
- mixed diet
- bowels: loose stools
- micturition: normal
- no known allergies
- no addictions
- AOM: 16yrs
- LMP: dec 4th
- TEMP: afebrile
- PR: 85 bpm
- RR: 18 cpm
- BP: 120/80 mmHg
- SPO2: 98% @ RA
- GRBS: 118 mg%
- pallor: +ve
- icterus: -
- clubbing: -
- cyanosis: -
- lymphadenopathy: -
- edema: -
- S1, S2 heard
- no thrills
- no murmurs
- BAE+
- NO DYSPNOEA
- NO WHEEZE
- CENTRAL POSTITON OF TRACHEA
- VESICULAR BREATH SOUNDS HEARD
- no added sounds
HEMOGRAM & CUE
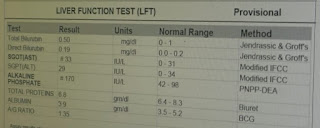
LFT & RFT
USG
CHEST X RAY
- INJ. METROGYL 500mg IV/ IM
- INJ. Pan 40 mg IV/ OD
- INJ. ZOFER 4mg IV/ OD
- Tab. ULTRACET PO/ BD
- Fluids NS @ 100 ml/ hr
- INJ. CIPROFLOXACIN 200mg IV/ BD
- Tab SPORLAC DS PO/ TID
- ORS sachets 200ml after each episode of stool (diarrhoea)

















.png)
.png)


No comments:
Post a Comment