🍁Greetings to one and all going through my E log!!
🩺This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment.
I am Nomika Alli (Roll no 179) of 8th Sem MBBS
A 65 year old male , daily wage laborer by occupation R/O Nalgonda came to the OPD on 12th August 2023 with complaints of involuntary movements of both limbs since 5 days.
History of present illness:
Patient is apparently asymptomatic 1 week back and then he had complaints of involuntary tonic clonic seizures of Bilateral upper and lower limbs, sudden in onset, lasting for 30 minutes associated with uprolling of eyelids, lateral tongue bite, deviation of mouth, frothing of saliva, urinary incontinence during episode.
Each episode often occurs in sleep after 1 hr of going to bed. Post ictal confusion present for 30 min after episode.
C/O Heaviness of head and dragging type of pain at frontal region.
C/O back pain and myalgia. Patient face appears to be dark and flushing during episode. Patient agitated and aggressive during and after episode for 30- 60 minutes.
No H/O chest pain, cough, fever, Shortness of breath
No H/O orthopnea, PND, sweating, Palpitation
No c/o Burning micturition, increased or decreased urine output
no c/o loose stools, nausea, vomiting
All throughout his illness, patient was able to carry his daily activities apart the episode duration.
His daily routine is waking up at 6: 00 am, drinks tea at 7:00 am, breakfast as rice and curry at 9:00 am and leaves for work. He used to have his lunch as rice and curry at 2: 00 pm and return to home by 6:00pm. He usually haves his dinner as rice and curry at 9:00pm and goes to bed by 10:00 pm.
History of past illness:
H/o exact complaints 1 year back a/o facial puffiness and pedal edema. He was bought to KIMS, Nkp. and given medication and asked to use medication regularly. But the patient stopped the medication after using it for 6-7 months (thought that symptoms subsided).
N/K/C/O DM, HTN, TB, Asthma, CAD, CVD
No Surgical History
PERSONAL HISTORY:
Diet: Mixed
Appetite: Normal
Sleep: adequate
Bowel and bladder movements: Regular
Addictions: 2-3 Beedi / day since 40 years
Allergies: no known
FAMILY HISTORY:
N/K/C/O HTN, DM, TB, Asthma, CAD, CVD, Epilepsy
GENERAL EXAMINATION:
Patient is conscious, coherent, cooperative to time, place and person.
Ht: Wt:
No signs of pallor,
no icterus,
no clubbing,
no cyanosis,
no koilonychia,
no lymphadenopathy,
no edema
vitals: temp: afebrile
BP: 130/70 mmHg
HR: 82bpm
RR: 20cpm
SpO2: 98%
SYSTEMIC EXAMINATION:
CNS: Conscious and normal speech
no neck stiffness
negative kernig's sign
Cranial nerves: normal
motor and sensory are normal
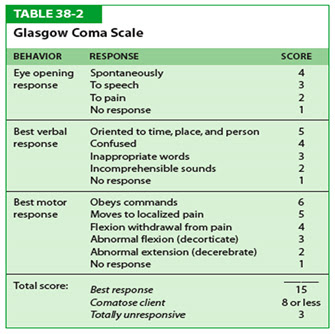
Glassgow scale score: 15
E4V5M6: Spontaneous eye opening,
orientated verbal response and
obey commands.
.jpg)
.png)
.jpeg)
.jpeg)
.jpeg)
.jpeg)
.jpeg)
.jpeg)

.jpeg)

.jpeg)
.jpeg)
.jpeg)
.png)
.png)


No comments:
Post a Comment